Bone repair remains a significant challenge in medical science due to the complexity of bone tissue, which must balance strength, flexibility, and biological integration. Fractures, bone defects from trauma, or diseases like osteoporosis and bone cancer often require advanced interventions to restore function. Traditional methods, such as autografts (using a patient’s bone) or allografts (donor bone), have limitations like limited supply, risk of rejection, or prolonged recovery times. The advent of 3D printing, coupled with innovative biomaterials like nano hydroxyapatite (nHA), offers a groundbreaking approach to overcoming these hurdles. 3D printing allows for precise, patient-specific designs, while nHA mimics the natural composition of bone, promoting regeneration.
This blog post explores how the synergy of 3D printing and nHA is poised to revolutionize bone repair. By enabling the creation of customized, biocompatible scaffolds, this technology addresses the shortcomings of traditional methods, offering faster healing, reduced complications, and improved outcomes.
At Heeger Materials Inc., we specialize in high-quality ceramic products with various materials and specifications, ensuring optimal performance for industrial and scientific applications.
Understanding Nano Hydroxyapatite
1. What is Hydroxyapatite?
Hydroxyapatite (HA) is a naturally occurring mineral form of calcium apatite, with the chemical formula Ca₁₀(PO₄)₆(OH)₂. It is the main inorganic component of bones and teeth (making up about 70% of bone and 90% of tooth enamel by weight).
2. What is Nano Hydroxyapatite (nHA)?
Nano hydroxyapatite refers to hydroxyapatite particles that are nanometer-sized (typically between 1–100 nm). Due to their tiny size, these particles have:
- Higher surface area
- Improved solubility
- Enhanced bioactivity (better interaction with biological tissues)
3. Properties of Nano Hydroxyapatite
Nano hydroxyapatite (nHA) is a calcium phosphate compound with a chemical composition (Ca₁₀(PO₄)₆(OH)₂) nearly identical to the mineral component of human bone and teeth. At the nanoscale, hydroxyapatite particles exhibit unique properties, such as increased surface area and enhanced bioactivity, making them ideal for medical applications. nHA’s biocompatibility ensures it integrates seamlessly with living tissue, promoting cell adhesion, proliferation, and differentiation, which are critical for bone regeneration.
- Biocompatible: Safe for use in the human body.
- Osteoconductive: Supports bone growth.
- Non-toxic & Non-inflammatory: Suitable for medical and dental applications.
- High mechanical strength (when used in composites).
4. Applications of Nano Hydroxyapatite
A. Dentistry
- Tooth Remineralization: Helps repair early cavities by depositing minerals on enamel.
- Dentifrices (Toothpaste): Used in some advanced toothpastes (e.g., Apagard, Boka) to strengthen enamel.
- Dental Implants & Bone Grafts: Promote jawbone regeneration.
B. Orthopedics & Bone Repair
- Bone Grafts & Scaffolds: Used in fractures, osteoporosis, and reconstructive surgery.
- Coatings for Implants: Enhances integration of metal implants (e.g., hip replacements) with bone.
C. Drug Delivery
- Acts as a carrier for controlled release of drugs (e.g., antibiotics, anticancer agents).
D. Cosmetics & Skincare
- Used in anti-aging creams (stimulates collagen production).
- Helps in skin repair and wound healing.
E. Water Treatment
- Removes heavy metals (e.g., lead, cadmium) due to its high adsorption capacity.
5. Advantages of Nano Hydroxyapatite
The advantages of nHA are numerous. Its nanoscale size allows for better penetration into biological systems, improving interaction with osteoblasts (bone-forming cells). Additionally, nHA is biodegradable, gradually dissolving as new bone forms, eliminating the need for surgical removal. It also supports angiogenesis (blood vessel formation), which is essential for delivering nutrients to healing tissues.
Property | Description | Benefit for Bone Repair |
Biocompatibility | Chemically similar to bone mineral | Reduces rejection risk |
Nanoscale size | High surface area, enhanced bioactivity | Promotes cell growth |
Biodegradability | Dissolves as bone regenerates | No need for removal |
Osteoconductivity | Supports bone cell attachment | Enhances regeneration |
6. Comparison with Conventional Hydroxyapatite
Property | Nano Hydroxyapatite | Regular Hydroxyapatite |
Surface Area | Very High | Lower |
Solubility | Higher | Lower |
Bioactivity | Enhanced | Moderate |
Remineralization | Faster & More Effective | Slower |
Looking for high-quality ceramic products? Explore Heeger Materials' selection.
The Role of 3D Printing in Bone Repair
3D printing (additive manufacturing) has revolutionized bone repair by enabling the fabrication of customized, patient-specific scaffolds, implants, and grafts with precise geometries and controlled porosity. When combined with biomaterials like nano hydroxyapatite (nHA), 3D printing offers advanced solutions for bone regeneration.
1. Why 3D Printing for Bone Repair?
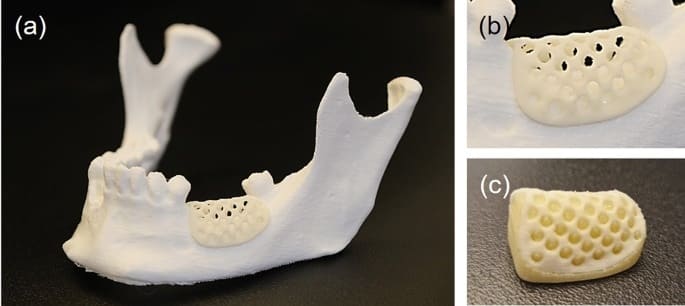
3D printing, or additive manufacturing, has transformed medical applications by allowing the creation of complex, patient-specific structures layer by layer. In bone repair, 3D printing is used to fabricate scaffolds—porous structures that support bone growth while providing mechanical stability. These scaffolds can be tailored to match the exact shape and size of a patient’s bone defect, ensuring a perfect fit and optimal integration.
Traditional bone grafts (autografts, allografts) have limitations:
- Limited supply (autografts require a second surgery).
- Risk of rejection or infection (allografts/xenografts).
- Lack of personalized fit.
3D printing overcomes these issues by:
✔ Customization – Matches the patient’s exact bone shape.
✔ Controlled porosity – Mimics natural bone structure for cell growth.
✔ Incorporation of bioactive materials (e.g., nHA, growth factors).
✔ Reduced surgery time & improved healing.
2. How 3D Printing Works for Bone Repair
A. Common 3D Printing Techniques
Method | How It Works | Materials Used | Best For |
Fused Deposition Modeling (FDM) | Extrudes melted polymer filaments | PLA, PCL, composites | Low-cost prototypes |
Stereolithography (SLA) | UV-cured liquid resin | Photopolymers, ceramics | High-detail scaffolds |
Selective Laser Sintering (SLS) | Laser fuses powder particles | PCL, HA, metals (Ti) | Strong porous implants |
Bioprinting (Extrusion-based) | Deposits bioinks (cells + hydrogels) | Alginate, collagen, nHA | Cell-loaded grafts |
B. Key Materials Used in 3D-Printed Bone Scaffolds
- Polymers (PCL, PLA, collagen) – Provide structural support.
- Ceramics (nano hydroxyapatite, β-TCP) – Enhance bone bonding.
- Composites (nHA + polymers) – Combine strength & bioactivity.
- Metals (Titanium) – For load-bearing implants.
3. Applications in Bone Repair
A. Patient-Specific Bone Implants
- Cranial/facial reconstruction – Custom skull plates.
- Dental bone grafts – Jawbone regeneration.
- Spinal fusion – 3D-printed interbody cages.
B. Porous Scaffolds for Bone Regrowth
- Mimics trabecular bone structure (~300–500 µm pores).
- Allows vascularization & cell migration.
C. Drug-Eluting Bone Grafts
- Controlled release of antibiotics (e.g., for osteomyelitis).
- Growth factors (BMP-2) to accelerate healing.
D. Bioprinted Bone Tissue
- Cell-laden bioinks (stem cells + nHA) for live grafts.
- Future potential: 3D-printed living bone.
4. Advantages of 3D-Printed Bone Repair
✅ Precision – Matches patient anatomy (CT/MRI-based design).
✅ Faster healing – Optimized porosity enhances cell growth.
✅ Reduced rejection risk – Biocompatible materials (nHA, PCL).
✅ Cost-effective long-term – Fewer complications vs. traditional grafts.
Explore our optimized ceramic products.
Synergy of 3D Printing and Nano Hydroxyapatite
The combination of 3D printing and nHA creates a powerful platform for bone repair. nHA is incorporated into 3D printing materials, such as polymer or ceramic composites, to produce scaffolds that are both mechanically robust and biologically active. The 3D printing process allows for precise control over the scaffold’s porosity, ensuring optimal cell infiltration and nutrient flow, while nHA enhances bone cell attachment and growth.
Studies have shown that nHA-enhanced 3D-printed scaffolds significantly improve bone regeneration compared to traditional materials. For example, a 2023 study demonstrated that nHA-based scaffolds led to faster bone formation in animal models, with new bone tissue forming within weeks. The synergy also allows for the inclusion of growth factors or drugs within the scaffold, further promoting healing.
Feature | 3D Printing Contribution | nHA Contribution |
Customization | Patient-specific designs | Enhances biological integration |
Porosity | Controlled pore size for cell growth | Promotes osteoconductivity |
Mechanical Strength | Robust scaffold structure | Adds bioactivity without compromising strength |
Discover our high-quality ceramic materials.
Advantages Over Traditional Bone Repair Methods
Traditional bone repair methods, such as autografts, allografts, and synthetic grafts, have significant drawbacks. Autografts, while biocompatible, require harvesting bone from the patient, leading to additional surgery and pain. Allografts carry risks of immune rejection and disease transmission. Synthetic grafts, like metal implants, often lack biological integration, leading to long-term complications.
1. Personalized Implant Design vs. "One-Size-Fits-All" Grafts
Traditional Methods | 3D-Printed nHA Scaffolds |
- Autografts require a second surgery, causing donor-site pain. | ✅ Fully customized to match patient anatomy (CT/MRI-based). |
2. Enhanced Bone Regeneration vs. Passive Implants
Traditional Methods | 3D-Printed nHA Scaffolds |
- Metal implants (e.g., titanium) are bioinert, limiting bone bonding. | ✅ nHA is osteoconductive, accelerating bone growth. |
3. Reduced Complications & Infections
Traditional Methods | 3D-Printed nHA Scaffolds |
- Allografts risk disease transmission. | ✅ Antibacterial nHA coatings reduce infection risks. |
4. Mechanical Strength & Load-Bearing Capabilities
Traditional Methods | 3D-Printed nHA Scaffolds |
- Polymers alone are too weak for load-bearing bones. | ✅ nHA reinforces polymers (e.g., PCL, PLA) for bone-like strength. |
5. Cost & Surgical Efficiency
Traditional Methods | 3D-Printed nHA Scaffolds |
- Autografts require additional surgery. | ✅ Single-step implantation reduces OR time. |
Request a custom quote for high-quality ceramic materials.
Challenges and Limitations
Despite its promise, 3D printing with nHA faces several challenges. Technically, achieving consistent material properties, such as uniform nHA dispersion in the printing material, can be difficult. Printing resolution must also be optimized to create scaffolds with the ideal pore size for bone growth. Additionally, the mechanical strength of nHA-based scaffolds may not yet match that of metal implants for load-bearing applications.
Regulatory and ethical considerations are also significant. The approval process for new biomaterials and 3D-printed implants is rigorous, requiring extensive testing to ensure safety and efficacy. Ethical concerns, such as equitable access to advanced treatments, must also be addressed. Finally, large-scale clinical adoption is limited by the need for specialized equipment and trained personnel.
Challenges:
- Material consistency: Ensuring uniform nHA distribution.
- Printing resolution: Achieving optimal pore sizes for cell growth.
- Regulatory hurdles: Lengthy approval processes for new biomaterials.
- Accessibility: High costs and need for specialized expertise.
Future Prospects
The future of 3D printing with nHA is bright, with potential applications in personalized medicine. Advances in imaging and printing technologies could enable real-time scaffold production during surgery, tailored to the patient’s exact needs. Additionally, ongoing research into nHA formulations, such as doping with growth factors or antimicrobial agents, could further enhance scaffold performance.
Beyond bone repair, this technology could impact broader regenerative medicine fields, such as cartilage or organ repair. The ability to combine 3D printing with bioactive materials like nHA opens the door to fully regenerative implants that integrate seamlessly with the body, reducing the need for lifelong medical interventions.
Future Directions:
- Real-time printing: In-situ scaffold production during surgery.
- Enhanced nHA: Incorporation of growth factors or drugs.
- Broader applications: Extending to cartilage, dental, or organ regeneration.
At Heeger Materials Inc., we supply optimized-grade ceramic products that comply with ASTM and ISO standards, ensuring outstanding quality and reliability.
FAQ
Question | Answer |
What is Nano Hydroxyapatite (nHA), and how is it used in 3D printing? | Nano Hydroxyapatite is a bioactive material resembling human bone, and it's used in 3D printing to create customized bone scaffolds for repair. |
How does 3D printing with nHA improve bone repair? | 3D printing with nHA allows for precise, patient-specific bone scaffolds that enhance healing by mimicking natural bone structure and promoting regeneration. |
What are the advantages of using 3D printing for bone repair? | 3D printing provides customization, reduces surgical time, and offers better integration with natural bone tissue compared to traditional methods. |
Can Nano Hydroxyapatite be used for all types of bone injuries? | Nano Hydroxyapatite is particularly effective for treating small fractures, bone defects, and areas with limited healing potential, but its use may vary by case. |
Is 3D printing with nHA safe for patients? | Yes, Nano Hydroxyapatite is biocompatible and has been shown to promote bone healing, making it a safe choice for patients when properly applied. |
How is the 3D printing process for bone repair conducted? | The 3D printing process involves designing a scaffold based on patient scans, printing the nHA material, and implanting the scaffold into the damaged bone. |
The integration of 3D printing with nano hydroxyapatite represents a paradigm shift in bone repair. By combining the precision of 3D printing with the biocompatibility of nHA, this technology offers customized, regenerative solutions that outperform traditional methods. While challenges remain, ongoing advancements in materials science and printing technology are paving the way for widespread adoption.
The potential for personalized, efficient, and biologically compatible bone repair is within reach. Researchers, clinicians, and policymakers must collaborate to overcome technical and regulatory hurdles, ensuring this technology reaches those who need it most. The future of bone repair—and regenerative medicine as a whole—looks promising, with 3D printing and nHA leading the charge.
For top-quality ceramic materials, Heeger Materials provides tailored solutions for various applications.
Looking for premium ceramic products? Contact us today!


